The Shoulder
Distal clavicular osteolysis
Etiology - Pathology
Distal clavicle osteolysis is a pathologic process involving resorption of subchondral bone in the distal clavicle, which usually presents as pain localized to the acromioclavicular joint.
While the exact frequency has not been determined, distal clavicle osteolysis is believed to be an underdiagnosed disorder. More than 100 cases have been reported in US literature. The incidence has been increasing with the rapid growth in popularity of weight training in the past 20 years.
The etiology of distal clavicle osteolysis has been theorized differently. The first proposed etiology was that of an autonomic neurovascular origin, as one author noted the presence of ipsilateral anisocoria in 4 out of 8 patients. Another report proposed synovial invasion of the subchondral bone. Cahill noted the presence of microfractures in the subchondral bone in 50% of his series and proposed that repetitive microtrauma caused subchondral stress fractures and remodeling; this is the most accepted theory.
Usually there is disruption of articular cartilage, subchondral cyst formation, and evidence of increased osteoclastic activity.
Clinical
Patients invariably present with pain over the distal end of the clavicle and acromioclavicular joint (C-4 dermatome) the pain usually is described as a dull ache.
Patients with traumatic etiologies report a specific event as the start of their symptoms.
In patients with repetitive/overuse injuries, pain is exacerbated by athletic or work activity.
Weightlifters report most symptoms with bench press exercises.
On physical examination, patients have point tenderness over the affected acromioclavicular (AC) joint. The passive horizontal adduction movement elicits is the most painful movement. Crepitation may be present.
Radiology:
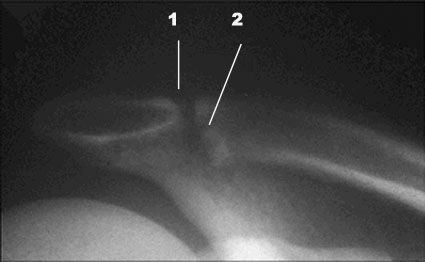 |
X-rays often appear normal in the early clinical course. With time, loss of subchondral bone detail in the distal clavicle, microcystic changes in the subchondral area (2), and widening of the AC joint (1) may be seen. |
Treatment
The natural history of the disease is that of a self-limiting disorder with resolution within 1-2 years with activity modification.
Conservative management consists of rest and avoidance of symptomatic activity. Steroid infltrations in the A-C ligaments are very helpful
Patients who fail conservative treatment or refuse to limit their activity are candidates for surgery.
The classic procedure for distal clavicle osteolysis is distal clavicle resection
Literature
| [Start] | [Main shoulder] | [Flowcharts shoulder] | [A System of Orthopaedic Medicine] |
Copyright © 2021 DR. L. OMBREGT All Rights
Reserved
The author can not be held responsible for any damage caused by the use of any information provided.